Malaria is a massive worldwide health problem. The Centers for Disease Control and Prevention estimate that 212 million cases of malaria occurred worldwide in 2015 and 429,000 of the infected people died.
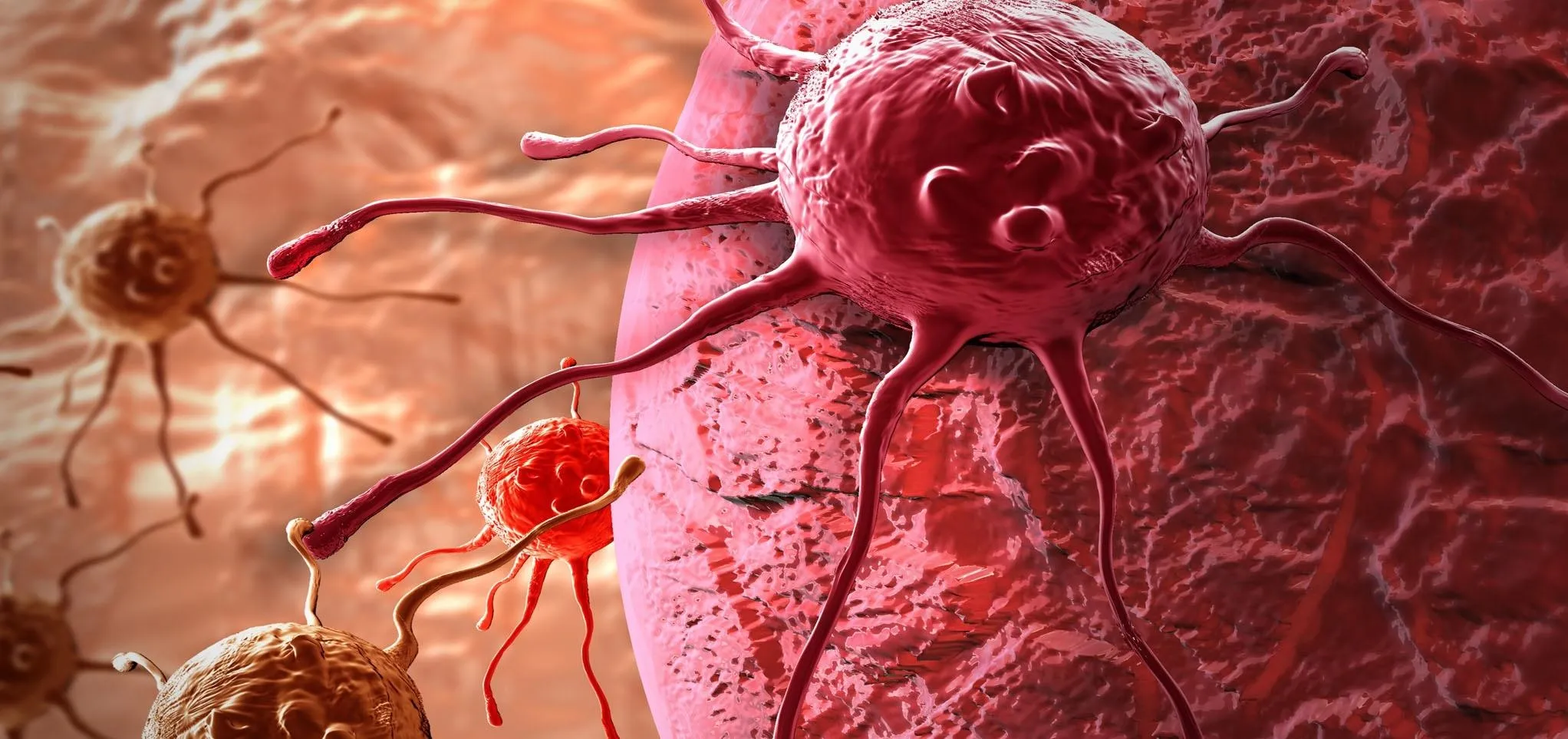
Once infected, the parasite multiplies in human red blood cells until it bursts out to infect more red cells. Researchers are targeting a key protein involved in this process, in an attempt to stop the parasite. They found that interfering with this protein slows the escape of the parasite from red blood cells, reducing the rate of infection and making it easier for the body to shut it down.
The research findings were published July 6 in PLOS Pathogens.
"Malaria parasites don't survive for long outside red blood cells, so if they get stuck on their way out, they might die before they have a chance to infect another cell," said Christine Collins, first author and researcher at the Francis Crick Institute.
Malarial Infections
Malaria is caused by the Plasmodium parasite, delivered by the bite of a female Anopheles mosquito that has previously dined on the blood from an infected person. Four kinds of malaria parasites infect humans: Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, and Plasmodium malariae.
The malarial parasite enters the body in the Sporozoite stage, where it invades the liver and develops into schizonts. Once mature, they burst from the liver releasing 2,000 to 40,000 parasites, each of which can infect a red blood cell. The merozoites use part of the red cell membrane to form a compartment called a vacuole, which protects them from proteins in the host red blood cell that might destroy the parasite. In the red cells, merozoites mature either into the sexual stage called a gametocyte — that can develop into an infectious sporozoite in an Anopheles mosquito — or into a schizont, which ruptures to release merozoites to infect more red blood cells.

The nine stages in the life cycle of the malaria parasite.
People infected with malaria experience symptoms associated with the reproductive stage of the parasite. When the parasites multiply in red blood cells, waste from the cells — such as hemozoin pigment and other toxic products — accumulates and is dumped into the bloodstream when the cell bursts, releasing more merozoites. The waste products stimulate the immune system to produce cytokines that cause fever and chills. Other symptoms of malaria are sweats, nausea, headache, and body aches. Usually, symptoms develop in 10 days to four weeks after infection.
Prevention relies on mosquito control and limiting exposure to the mosquitos that carry the malarial parasites, either by physical barriers like netting or by sprays containing DEET or another repellent. Travelers to some countries may be given medication to take to prevent malaria. These medications are the same as drugs used to treat malaria and include Atovaquone-proguanil, doxycycline, chloroquine, primaquine, or mefloquine.
Treatment is complicated by the fact that malarial parasites in some parts of the world are more likely to be drug-resistant. Plus, not all treatment medications can be taken by everyone — they have side effects, and pregnant women and people with glucose-6-phosphate dehydrogenase deficiency can't take primaquine.
Additionally, Plasmodium vivax and Plasmodium ovale parasites can stay dormant in the liver for several months up to about four years after initial infection. For reasons that remain unclear, the parasites can reactivate and start to invade red cells again, when that happens, the infected person relapses and experiences malaria symptoms again.
The sheer volume of infections and deaths highlight the importance of finding new ways to cure malaria infections. The research team from the Francis Crick Institute have figured out a way to interfere with an important step in the parasite's infectivity.
Stopping the Parasite in Its Tracks
The scientists already knew that when the malaria parasite escapes human red blood cells, it uses proteins to break through the vacuole they develop in, then the cell membrane.
"We focused on the most common protein, known as SERA5, assuming that it probably has an important role since there is so much of it," study researcher Mike Blackman, of the Francis Crick Institute, said in a press release.
SERA5 protein is found in the red blood cell compartment where the parasite grows. To test its role in malaria's spread to other red cells, the team genetically modified some malaria parasites to lack SERA5 and some to lack both SERA5 and SERA4 proteins. Once the modified parasites were allowed to infect red blood cells in test tubes, the researchers watched to see if the parasites lacking SERA proteins would be able to exit the red cells.

Time-lapse video shows that malaria parasites lacking SERA5 (right) break through membranes faster than normal (left) but many get stuck on their way out, meaning that they are less likely to invade other red blood cells.
They found the parasites lacking SERA5 and those lacking both SERA5 and SERA4, actually broke through the membranes faster than unmodified parasites, but many got stuck on their way out because the vacuole they were developing in and the cell membranes did not rupture properly. SERA5 was needed for the merozoites to disseminate to other red cells efficiently and without the protein, the parasite couldn't control the speed at which surrounding membranes enveloped it.
As for the future, the researchers think SERA5 might be a good target for new anti-malarial drugs. The researchers are already working with the pharmaceutical company, GSK to investigate the possibility.
- Follow Invisiverse on Facebook and Twitter
- Follow WonderHowTo on Facebook, Twitter, Pinterest, and Google+
Cover image by Steven Glenn/CDC





















Comments
Be the first, drop a comment!