Six people have died from fungal infections in Pittsburgh hospitals since 2014—that fact is indisputable. The rest of the situation is much vaguer. A lawsuit has been filed against the hospitals on behalf of some of the deceased patients, alleging that moldy hospital linens are to blame. While the lawyers argue over who's at fault, let's look at how this could have happened.
Five of the dead were patients in the transplant units at the Presbyterian and Montefiore campuses of the University of Pittsburgh Medical Center (UPMC) in Allegheny County, Pennsylvania. The sixth patient had leukemia and was receiving chemotherapy. He died in the ICU of Shadyside Hospital, also part of the UPMC, one day after developing a fungal pneumonia.
It's not entirely surprising that these two patient populations might get a fungal infection. People who have received a transplant take anti-rejection medications to help prevent their body from rejecting the new organ. Those medications decrease the overall activity of their immune system and makes them more susceptible to fungal infections. Likewise, chemotherapy drugs can also kill white blood cells, decreasing the body's ability to fight infections.
Overall, about 10% to 25% of patients with acute leukemia develop an invasive fungal infection, but the fatality rate is 50%—and up to 100% if the fungal infection reaches the blood or the patient doesn't have enough white blood cells to fight the infection. About 3% of transplant patients contract a fungal infection in the first year after the transplant.
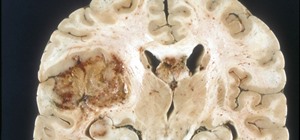
The twist to this story is that all the patients were hospitalized in facilities within the University of Pittsburgh Medical Center, and all contracted fungal infections with mucormycosis. Fungal infections in transplant patients are usually due to either Candida, Aspergillus, or Cryptococcus.
The Culprit
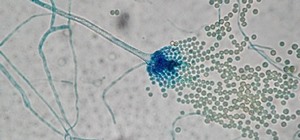
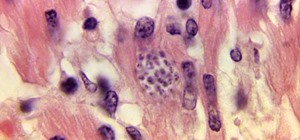
A report issued by the Pennsylvania Department of Health found that the first four patients were infected with different species of mucormycetes fungus, the group of fungi that causes mucormycosis. They identified Rhizopus oryzae (arrhizus), Rhizopus microsporus, and Lichtheimia corymbifera in three different patients, and another lab identified Lichtheimia fungal DNA in the fourth patient.
Mucormycetes fungi are found just about everywhere in nature, most commonly on decaying organic materials, like leaves and the familiar old bread mold. Spores on the tip of the growing fungus break off and transmit the fungus.
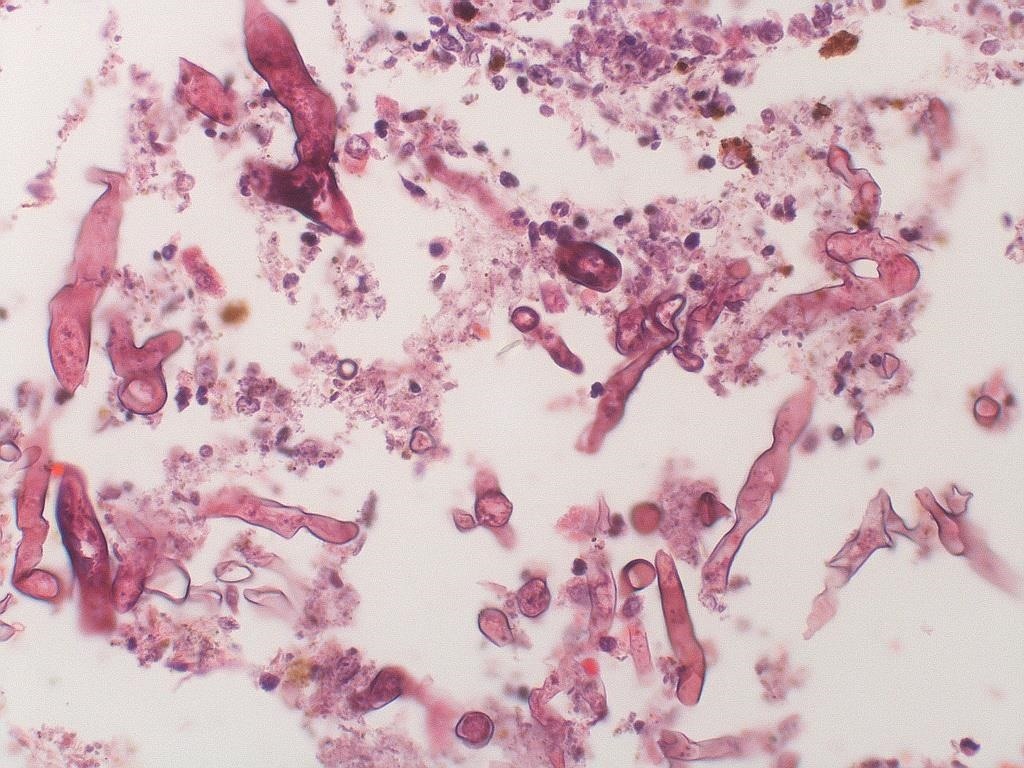
Mucormycosis is particularly deadly to people with compromised immune systems like those receiving chemotherapy or anti-rejection medications. About 50% of the people who contract mucormycosis die. According to the Centers for Disease Control and Prevention (CDC), inhalation of spores, or direct entry of spores through a wound, are the usual routes of infection with this type of mold.
The missing piece of this puzzle is how and where did these patients come in contact with mucormycetes? Could they all have been outside working in their garden and exposed to mucormycetes in the dead leaves there? It doesn't seem likely (since they were in the hospital), and that's what officials have been trying to figure out.
Experts Weigh In
In September of 2015, the CDC was notified of the possibility that the four cases known at that time represented an outbreak of mucormycosis. Their analysis of the cluster of cases considered several factors that could have played a role in the infections:
Three of the four patients had stayed in the same hospital room in one hospital. The patients had all been given voriconazole as treatment for the fungal infection—maybe it was contaminated. Past Rhizopus infections had been due to construction projects that spread spores, and there were multiple construction projects occurring at two of the hospitals. The patients had been housed in negative pressure rooms—rooms where the airflow is designed to flow into the room, but not out—preventing possible contagions from escaping the hospital room.
The CDC could not nail down a definitive source of the cluster of cases. They concluded their report by writing, "Caring for immunosuppressed patients in negative-pressure environments has been previously identified as a risk factor for invasive mold infections, possibly related to the potential to concentrate dust and mold spores in these rooms." But they stopped short of saying the infections were hospital-acquired or naming the precise source.
The UPMC commissioned hospital environmental specialists to inspect the Paris Healthcare Linen facility, the source of the hospitals' linens. The inspectors found wet sheets delivered to one of the hospital laundry areas had heavy fungus growth and they reported finding lint and mold near vents blowing air used to dry linens that went to UPMC facilities.
Hospitals, and the linens used by them, are bound by very strict accreditation standards and are regularly inspected for compliance with those standards. The Healthcare Laundry Accreditation Council requires accredited laundry facilities that process reusable textiles for healthcare organizations to maintain certain levels of cleanliness. The standards apply to the facilities, the processes, and the linens themselves. Laundries are inspected every three years to maintain their accreditation.
According to Paris Healthcare Linens, it is certified by the Healthcare Laundry Accreditation Council. Does that mean the linens delivered to the Pittsburgh hospitals were not contaminated? Not necessarily.
If the fungus did come from linens, it's not likely they would have been dangerous to a non-immune compromised person. The patients infected with fungus were very sick and had medical issues that made them extra sensitive to mold that doesn't affect the rest of us. That said, nobody wants moldy sheets or linens.
Mold's favorite places to grow are wherever it's warm, moist, and dark. It would not grow on dry, clean sheets, whether from a hospital laundry or in your own home, but it will grow on that wet beach towel you threw in the bottom of the closet and forgot about it. Any towel that sits around wet could potentially be growing unfriendly microbes, so hang them to dry and change them out frequently for clean ones. A good washing and thorough drying will help, and to get rid of mildew smell, add some bleach or white vinegar to the wash.
We may not be any closer to figuring this medical mystery out. In the end, the legal aspect of this matter will be decided in court. Preventing further infections will be responsibility of healthcare providers. The unfortunate truth is that the sickest patients are the most vulnerable to microbes the rest of us come in contact with every day.
Just updated your iPhone? You'll find new emoji, enhanced security, podcast transcripts, Apple Cash virtual numbers, and other useful features. There are even new additions hidden within Safari. Find out what's new and changed on your iPhone with the iOS 17.4 update.





















Be the First to Comment
Share Your Thoughts