The noses of kids who live in areas of intense pig farming may harbor antibiotic-resistant bacteria, presumably acquired from the animals, according to a new study by scientists at the Johns Hopkins Bloomberg School of Public Health, UNC Gillings School of Global Public Health, and Statens Serum Institut in Denmark, published in Environmental Health Perspectives.
Infections with drug-resistant microbes kill an estimated 700,000 people worldwide annually, and it's estimated that this number will increase to 10 million by 2050.
At least 2 million people in the US contract infections with drug-resistant bacteria every year, and about 23,000 of them die, according to the Centers for Disease Control and Prevention (CDC).
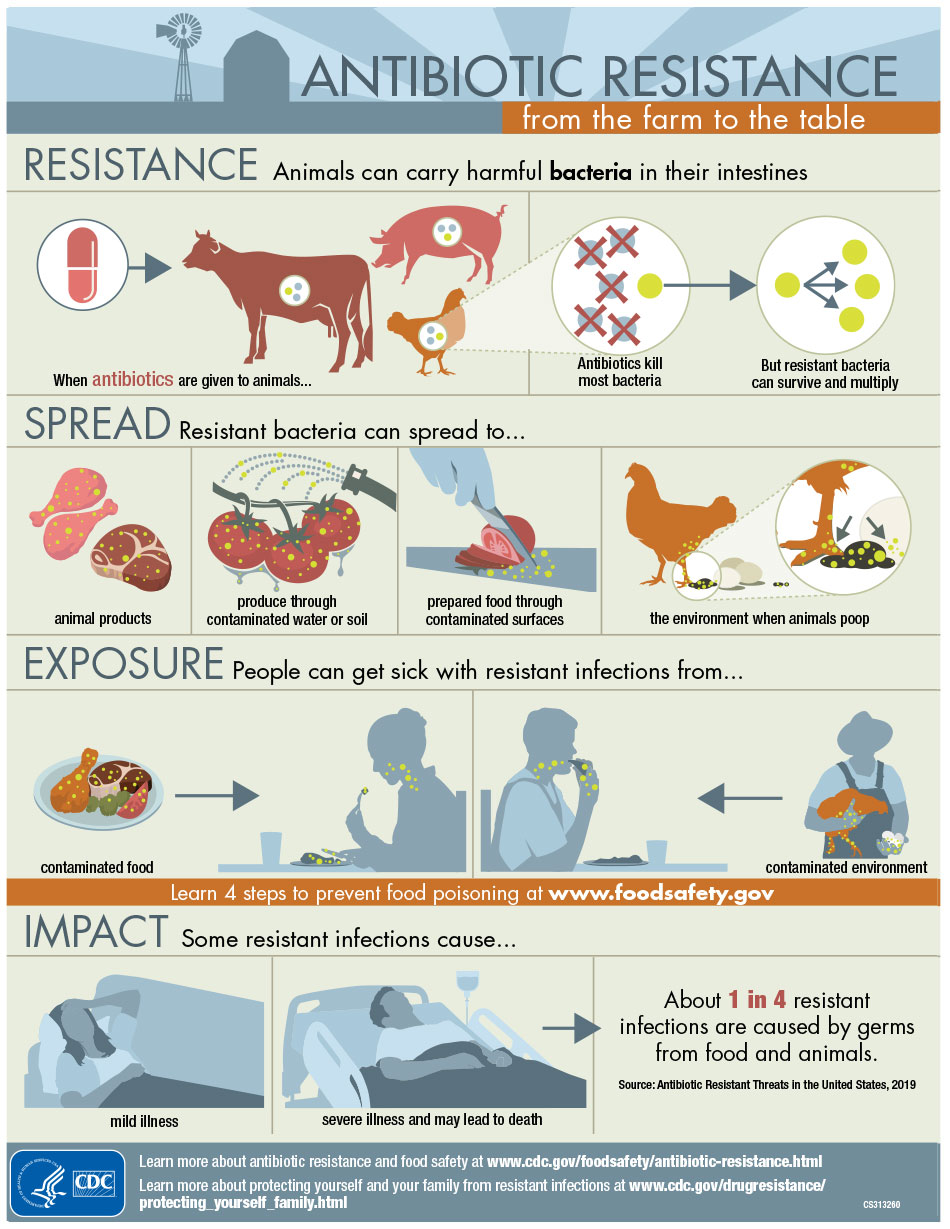
The kids in the recent study found with MRSA (methicillin-resistant Staphylococcus aureus) in their noses weren't sick, but they are a symptom of a broken farming system. The CDC has estimated that 20% of infections with drug-resistant organisms are caused by food and animals. The bacteria infect humans by contaminated food (handling and eating raw or undercooked and contaminated meat), drinking or swimming in water contaminated with animal feces, and contact with animals.
And now, just living near a farm could mean you're more likely to contract a dangerous antibiotic-resistant microbe.
The Other White Meat
Just like people, farmers treat infections in farm animals with antibiotics, but unlike people, farm animals are more apt to be given antibiotics prophylactically to prevent infections and to help the animals grow — because everybody wants a bigger chicken breast, right? And the amount of pork and chicken we eat in the US has increased steadily since 1990.
The use of penicillins, tetracyclines, and macrolide antibiotics (like erythromycin) on farms grew 26% from 2009 to 2015, according to the Food and Drug Administration (FDA). Those antibiotic treatments cause some of the microbes in chicken, pigs, and beef cattle to become resistant to them — and those are the same kind of antibiotics used in people — likely for similar infections.
In simplest terms, these resistant bacteria are no longer sensitive to most of the antibiotics available to treat them and are threatening the health of people worldwide.
Bacteria become resistant to antibiotics by repeated treatments with them. Farmers frequently treat animals with antibiotics, and the use of those antibiotics is linked to an increased threat of resistant microbes to humans. And now we know that people come into contact with these resistant microbes, including the MRSA in this study, just by living near farms.
The Nose Knows
The study analyzed parents and children in 400 households in an area of North Carolina with heavy pig farming. The study analyzed nasal swabs of 198 pig farmer parent and child pairs and 202 community family pairs. Those pairs included one child from each family under the age of seven.
The researchers tested for the presence of MRSA and MDRSA (multidrug-resistant Staphylococcus aureus) on the swabs. The children of pig farm workers were more than twice as likely to have their noses drug-resistant bacteria in their noses than other kids in the community.
About 14% of the hog farmers' kids had MRSA in their noses, and 23% carried MDRSA, compared to 6% of kids in the community carrying MRSA and 8% had MDRSA.
Bacteria in the nasal swabs of the adult pig workers and adults in the community were more similar than those of the young children. About 2% of adult pig workers and 3% of adults in the community had MRSA in their noses. The researchers found MDRSA in the noses of about 12% of adult pig farmers, compared to 8% of adults living in the community.
Since the types of bacteria in the noses of pig farming adults and their children were different, the researchers felt that the drug-resistant bacteria probably traveled to kids from clothes and equipment brought home from the pig worker parent parent-to-kid contact.
The FDA took measures in January of this year to limit some types of antibiotic use in farm animals. Guidance for Industry #213 is the culmination of a process that began in 2013 to eliminate the use of antimicrobial drugs with importance in human medical treatment in animals for purposes of growth production.
Until we figure out how to get the antibiotic resistance under control, breaking the chain of infection may be our next best bet. According to the new research, part of the chain now involves the snot of kids who live on and near pig farms.
- Follow Invisiverse on Facebook and Twitter
- Follow WonderHowTo on Facebook, Twitter, Pinterest, and Google+
Cover photo by Kanjanee Chaisin/123RF



























Comments
Be the first, drop a comment!