Usually, the mucus lining of the female genital tract presents a barrier that helps prevent infections. But, somehow, the bacteria that causes gonorrhea gets around and through that barrier to invade the female genital tract.
Scientist Liang-Chun Wang, from the Department of Cell Biology and Molecular Genetics at the University of Maryland, and colleagues, developed a new model to study how Neisseria gonorrhoeae infects female endocervical tissue and discovered the process the bacteria uses to penetrate the cells and cause an infection. Their work was just published online in PLOS Pathogens.
When most organisms enter the female reproductive tract, the infected cells in the lining of the female genital tract are shed and disposed of while keeping the tight connections between cells and the mucosal lining intact. The barrier remains unbroken.
The researchers used samples of endocervix tissue that they infected with N. gonorrhoeae in the lab to study how the bacteria gets around and through this normal process.
They found that the bacteria breaks connections between cells and causes cells to shed, while opening paths for penetration that allow it to adhere to and invade the cells of the lining. N. gonorrhoeae does this by activating and redistributing a protein called non-muscle myosin II, and by activating the movement of calcium into and out of the cells.

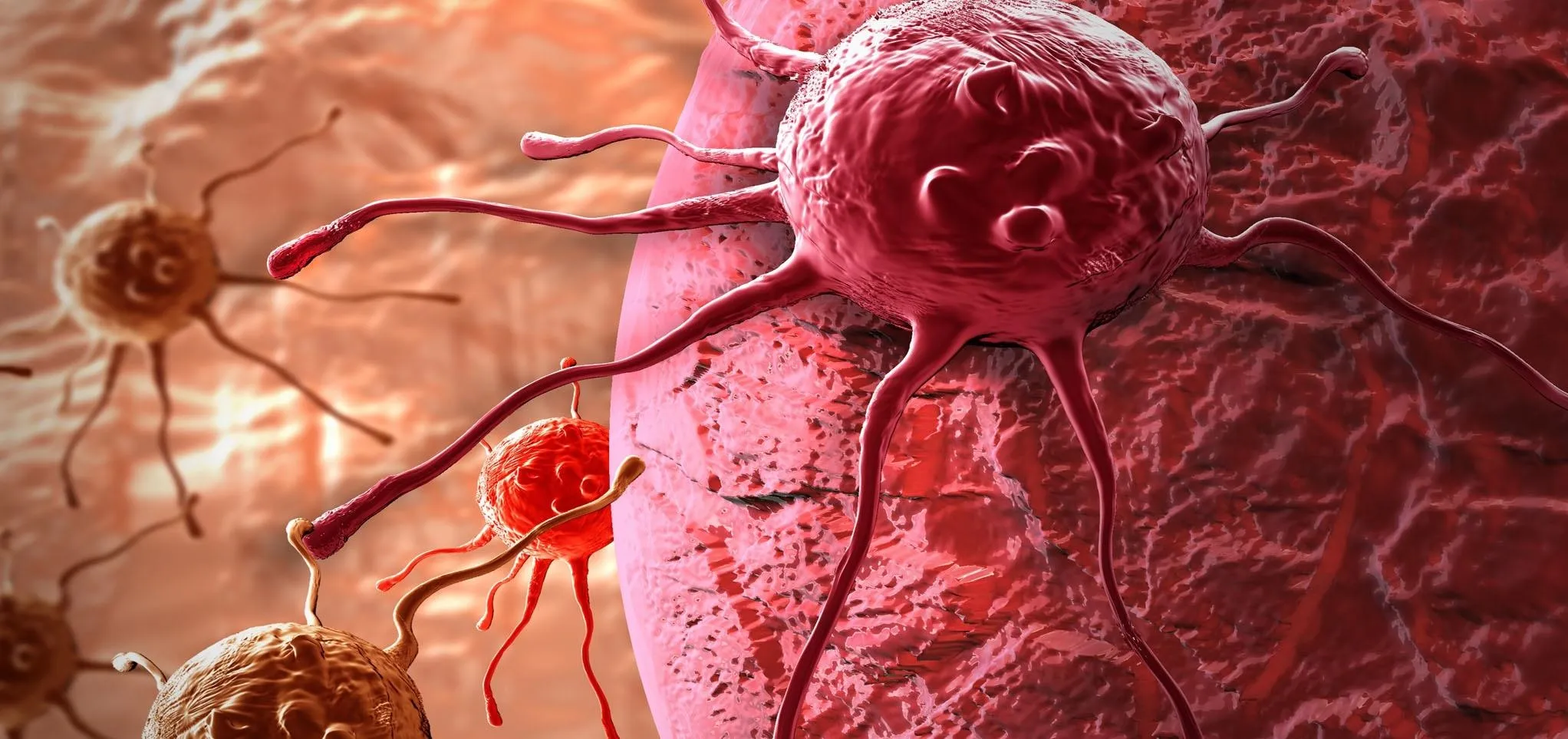
N. gonorrhoeae (in red) infection in the human endocervical tissue is visualized by immunofluorescence.
Further experiments showed that the bacteria can either promote or inhibit this penetration mechanism, depending on which of the bacteria's genes are expressed at that time.
The new study represents the first time researchers have demonstrated in the lab how N. gonorrhoeae penetrates the female endocervical tissue and provides us with a mechanism and genes that can be targeted to help stop the process.
Gonorrhea—A Problem That's Not Going Away
Gonorrhea is the second most commonly reported notifiable disease in the US—cases of the disease must be reported to the Centers for Disease Control and Prevention (CDC).
It looked like we were getting on top of the number of gonorrheal infections in the US until 2009, when the previously declining rates started to increase again.
The rate of gonorrhea cases reported to the CDC increased 12.8% from 2014 to 2015, and increased 19.9% from 2011 to 2015. More women younger than age 25 have gonorrhea than men.
It's fairly common for gonorrhea to cause no symptoms, especially in women. If symptoms do develop, it can take from two to five days after exposure, and they may even show up to 30 days later.
When an infected woman does have symptoms, she may experience painful or burning sensation when urinating, increased vaginal discharge, and vaginal bleeding between periods. But women who don't know they have gonorrhea because they have no symptoms don't seek treatment and gonorrheal infections are a major cause of pelvic inflammatory disease.
In pelvic inflammatory disease the infection causes inflammation of the uterus, ovaries, and other female reproductive organs. That inflammation causes scarring of those organs that can lead to very serious problems, such as infertility caused by damage to fallopian tubes, ectopic pregnancy, abscesses, and chronic pelvic pain.
Unlike some superbugs, gonorrhea is still treatable with antibiotics, even after it causes pelvic inflammatory disease—although not all the damage may be reversible. Antibiotic resistance is increasing, but about 60% of the infections are still treatable with penicillin, tetracycline, ciprofloxacin, or some combination of those drugs.
We need to attack the growing problem from every angle—prevention, detection, and treatment—to get the infection rates to decline again.
The more we learn about the processes N. gonorrhoeae uses to set up infections—like the new research by Liang-Chun Wang and colleagues, the better equipped we are to find new ways to fight them.
- Follow Invisiverse on Facebook and Twitter
- Follow WonderHowTo on Facebook, Twitter, Pinterest, and Google+
Cover image by James Archer/CDC






















Comments
Be the first, drop a comment!