A terrifying antibiotic-resistant superbug, one thought to only infect hospital patients, has made its debut in the real world. For the first time ever, the superbug carbapenem-resistant Enterobacteriaceae (CRE) infected six people who hadn't been in or around a hospital in at least a year, and researchers aren't sure how they got infected.
The outlook for these infections wouldn't be so scary if they could easily be treated with antibiotics. But what makes some members of the Enterobacteriaceae family so scary is that they are rapidly becoming resistant to most types of antibiotics. They survive and grow despite treatment with most antibiotics. They have become superbugs.
To make matters worse, these superbugs usually infect patients in hospitals and nursing homes. Bacteria live in hospitals, and despite healthcare workers best efforts, patients who were not infected before admission can actually get infected while they are patients. And bacteria in hospital settings are more likely to be resistant to antibiotics.
That's why finding CRE infections in the community is troubling. Clearly, the superbugs are not confined to hospitals anymore and they are infecting people who are not hospitalized. A double whammy.
Who Are the Superbugs?
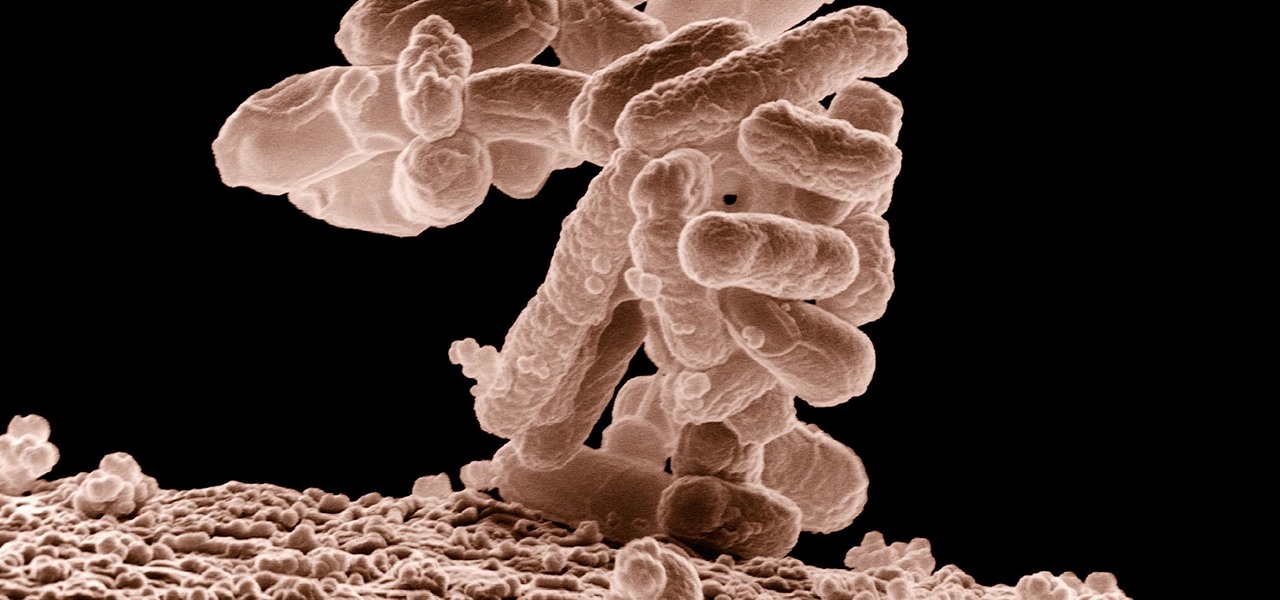
The CRE superbug is an Enterobacteriaceae, a common bacteria in the human intestines. You've probably heard about other bacteria in the Enterobacteriaceae family, such as Klebsiella, E. coli, Salmonella, and Shigella.
Enterobacteriaceae doesn't usually cause disease. Sometimes, though, if they spread outside the body, the bacteria can infect wounds, or cause urinary tract infections, blood infections, and pneumonia. The bacteria can be spread from person to person through contact with infected people or through contaminated medical devices, such as catheters or ventilators.
What makes the bacteria super is when it becomes immune to the effects of antibiotics. It doesn't die after treatment with the usual antibiotic prescribed for the infection. And often it becomes resistant to most antibiotics that could be used to treat it.
Carbapenem-resistant Enterobacteriaceae is joining the ranks of methicillin-resistant Staphylococcus aureus (MRSA) as scary superbugs. The other four superbugs named by the Centers for Disease Control and Prevention (CDC) as health threats are: ESBL-producing Enterobacteriaceae, vancomycin-resistant Enterococcus, multidrug-resistant Pseudomonas aeruginosa, and multidrug-resistant Acinetobacter.
Superbugs have become a real problem in healthcare settings because the bacteria are likely to be found there, patients are easier to infect because they are already sick, and they are very difficult to treat.
The CDC estimates that one in seven hospital-acquired catheter and surgery infections are due to one of the six antibiotic-resistant bacteria. For long-term care facilities, the number rises to one in four hospital-acquired infections due to antibiotic-resistant superbugs.
It has been projected that by 2050, antibiotic-resistant superbugs could kill ten million people a year.
How Superbugs Become 'Super'
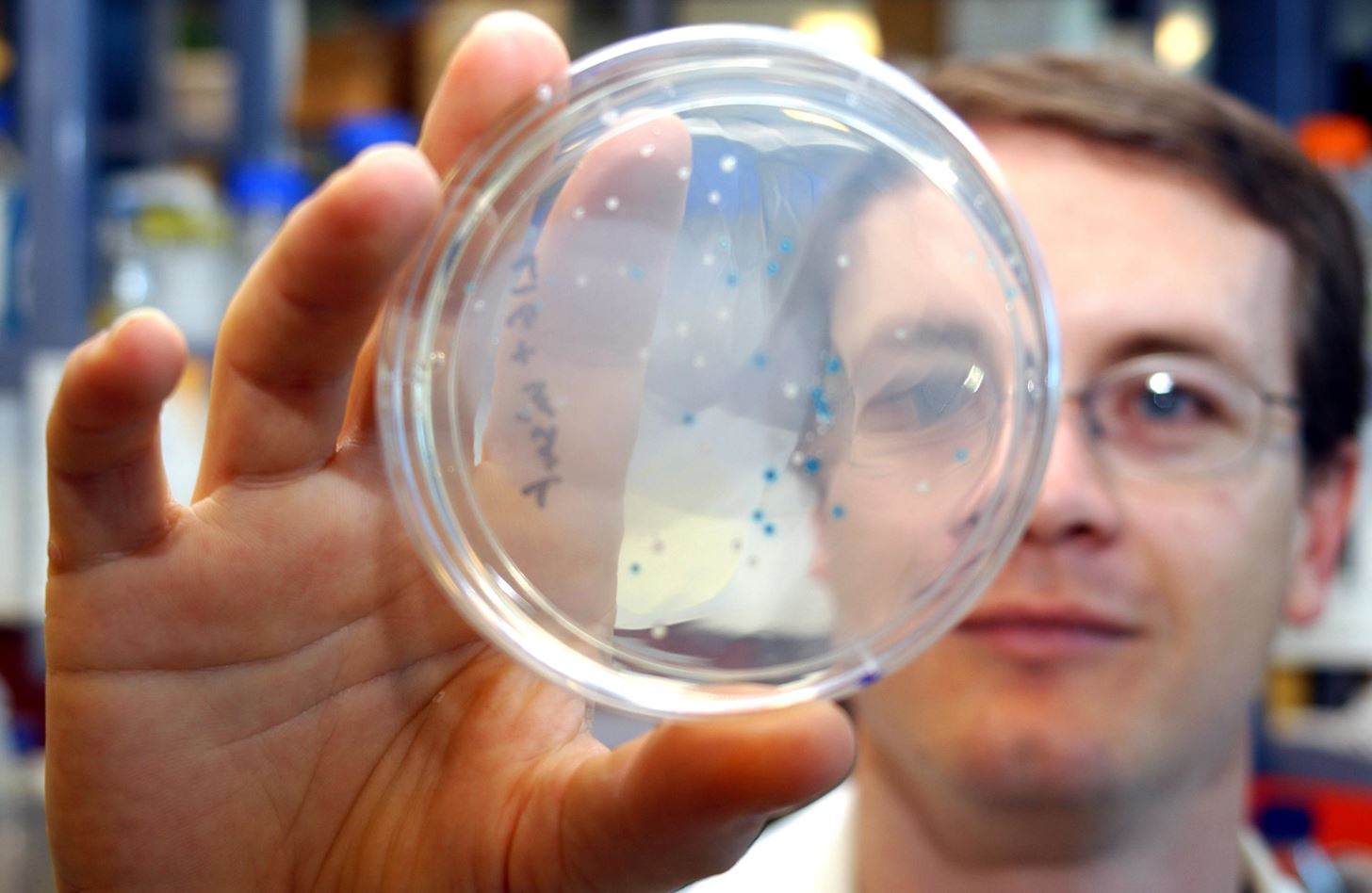
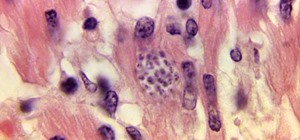
How does antibiotic resistance happen? Bacteria multiply rapidly. Some types of E. coli double in number every 20 minutes. That means in 24 hours, a single bacteria can become 4,722,366,482,869,645,213,696 bacteria. During this rapid multiplication, genetic mutations occur. If the mutation gives the bug an advantage—for example, the ability to survive antibiotics, those strong bugs will live on and multiply. Soon, most of the bacteria will be antibiotic resistant and we'll have a problem.
A recent study out of the University of Copenhagen, published in the December 16 issue of the journal Science, found that some bacteria can also survive antibiotic treatment by reprograming themselves into "persister cells" and enter a type of hibernation—in that state they can tolerate antibiotic treatment without dying. Later, they can resuscitate themselves and live on normally.
Resistance genes can also spread between bacteria—traits can be traded between individual bacteria, and even between species, on plasmids, small circles of DNA that code for specific proteins and enzymes. In this case, the bacteria developed an enzyme that inactivated carbapeneum. That made the Enterobacteriaceae resistant to the antibiotic effects of carbapeneum.
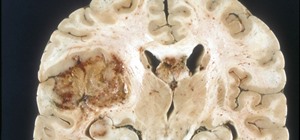
The bad news for people infected with CRE is that the bacteria was already resistant to cephalosporins, and carbapeneum was considered the last-ditch antibiotic. A study of patients at Cleveland Clinic in Ohio found that only 42% of patients with carbapenem-resistant Klebsiella pneumoniae bloodstream infections survived their hospital stay.
Help Protect Yourself
The best way to deal with CRE—or any antibiotic-resistant bacteria—is to not become infected in the first place. The CDC list these steps you can take to protect yourself:
- Tell your doctor if you have been hospitalized.
- Take antibiotics only as prescribed.
- Expect all doctors, nurses, and other healthcare providers to wash their hands with soap and water or an alcohol-based hand rub before and after touching your body or tubes going into your body. If they do not wash their hands, ask them to do so.
- Clean your own hands often, especially before preparing or eating food, before and after changing bandages, after using the bathroom, and after blowing your nose, coughing, or sneezing.
Setting the new report of CRE in the community aside, one way to fight superbugs is to decrease the hospital-acquired infection rate. Strict hospital hand-washing and other infection control measures have worked to reduce inpatient infections. The CDC reported that these precautions caused a 50% decrease in blood infections between 2008 and 2014 in patients with a catheter in their vein, and a 17% decrease in surgical site infections during the same time period.
Fighting Superbugs
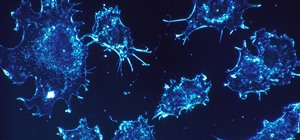
Researchers have looked to other bacteria for help in the fight against antibiotic-resistant bacteria. Bdellovibrio bacteriovorus is a microscopic predator that looks for and eats its own kind. Scientists put it together with a diarrhea-causing Shigella bacteria to see if the Bdellovibrio would kill it.
The Bdellovibrio decreased the Shigella population 4,000-fold. Next, the researchers infected zebrafish larvae with Shigella, then gave them Bdellovibrio. About 60% of the zebrafish larvae lived. This is great news for zebrafish, but a lot more work has to be done before anyone can say if this will be a useful treatment for humans.
Researchers at the Massachusetts Institute of Technology (MIT) are also trying to use biological systems to kill bacteria instead of antibiotics. In a 2015 American Chemical Society publication, they described a method they developed to infect the bacteria with DNA molecules called plasmids. The plasmids then expressed different proteins from within the bacteria cell that killed the bacteria. The novelty of this system is that the bacteria did not burst. A massive burst of dead bacteria can overwhelm the body and cause death.
The scientific jury is still out as to the reason and significance of finding CRE infections outside of hospital settings. The good news is that the medical and research communities are reaching deep into their bag of tricks to try to beat these bugs at their own game.
Just updated your iPhone? You'll find new emoji, enhanced security, podcast transcripts, Apple Cash virtual numbers, and other useful features. There are even new additions hidden within Safari. Find out what's new and changed on your iPhone with the iOS 17.4 update.




















Be the First to Comment
Share Your Thoughts