The search is on to find antibiotics that will work against superbugs — bacteria that are rapidly becoming resistant to many drugs in our antibiotic arsenal.
By carefully choosing antibiotics that killed bacteria in different ways, a team of researchers found that combinations of three antibiotics — ones that are ineffective against superbugs when used alone — were capable of killing some of our worst antibiotic-resistant bacteria.
Researchers describe the antibiotic combo treatment in two research papers, one published in the May issue of the Journal of Antimicrobial Chemotherapy, and the other in the in the April issue of Antimicrobial Agents and Chemotherapy.
The Urgent Threat
So many bacteria are becoming resistant to so many antibiotics that both the World Health Organization and the Centers for Disease Control and Prevention (CDC) have published lists of those microbes that pose the most urgent threats to global health.
Enterobacteriaceae, the family to which Klebsiella pneumonia belongs, has the dubious honor of attaining CDC's highest threat level — "urgent threat." Klebsiella shares this threat level with Neisseria gonorrhoeae and Clostridium difficile. CDC defines urgent threats as infections with high consequences across several criteria, like severely dwindling options for treatment and high death rate. Bacteria in this category have the potential to become widespread.
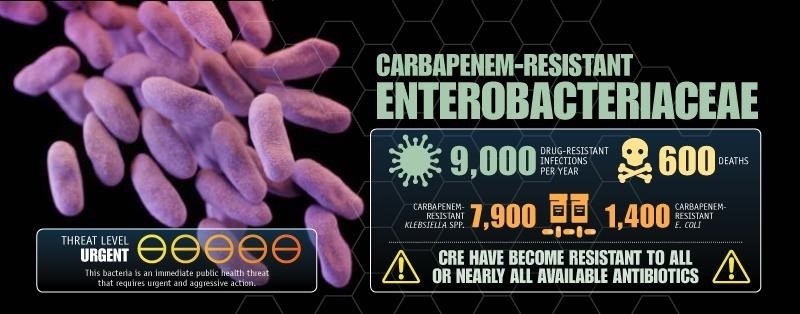
Carbapenem-resistant Enterobacteriaceae infections are becoming more frequent in hospitalized patients, are resistant to all or nearly all treatment options, and almost half the people whose blood becomes infected with these organisms die.
Multi-drug resistant Acinetobacter falls into CDC's second highest level of threat, "serious threats." This level includes bacteria for which there are still some antibiotic treatment options and they occur at a relatively low frequency in the US. Others in this category include Pseudomonas aeruginosa, Salmonella, and Multi-drug resistant Staphylococcus aureus (MRSA), to name a few.
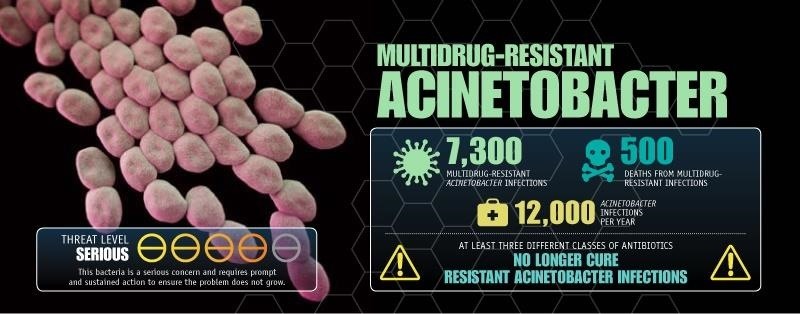
Acinetobacter causes pneumonia or bloodstream infections, often in already critically ill patients. Many of these bacteria are very resistant to antibiotics.
The Infectious Diseases Society of America has dubbed a subset of these antibiotic resistant bacteria ESKAPE pathogens — because the group includes Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species.
But the biggest threat of all is the collective threat these bacterial infections pose. Economist Jim O'Neill, appointed by British Prime Minister David Cameron to head a review of antimicrobial resistance estimated that antimicrobial resistance will kill 10 million people a year by 2050.
"These bacteria are extremely problematic and have become resistant to nearly all available antibiotics. We needed to think differently to attack this problem," said Brian Tsuji, a researcher at the University of Buffalo and author of both studies.
The Triple Antibiotic Trick
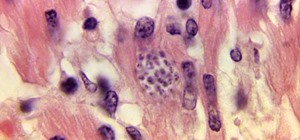
The new research employed a unique strategy to fight antibiotic resistance. The researchers used a trio of antibiotics, choosing each to complement the other, building a combination that would kill the bacteria through different mechanisms, hopefully resulting in an outsized effect than the three alone. They evaluated their drug combinations on two tough bacteria: Acinetobacter baumannii, described in the paper by first author Justin Lenhard, and Klebsiella pneumoniae in research led by Zackery Bulman, both from the University of Buffalo.
The researchers tested combinations of polymyxin B, meropenem, and ampicillin-sulbactam against Acinetobacter baumannii. They treated Klebsiella pneumoniae with a combination of polymyxin B, meropenem, and rifampin.
They tested drug combinations on bacterial samples in the lab individually, in pairs, and in triple combinations. The researchers evaluated the time it took the antibiotics to kill the bacteria and the time it took for them to regrow if the treatment didn't entirely kill them.
None of the antibiotics used alone were able to kill Acinetobacter baumannii, and only the pair of polymyxin B and meropenem was able to kill the bacteria effectively, but the bacteria regrew in three days.
The triple combination was about as effective at killing Acinetobacter baumannii as the pair of polymyxin B and meropenem, but triple treatment prevented regrowth of the bacteria.
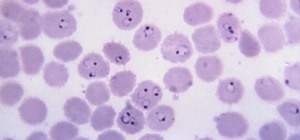
The most effective double combination treatment of Klebsiella pneumoniae was polymyxin B and rifampin. In about 30 hours the bacteria regrew to original levels.
The triple combination of polymyxin B, meropenem, and rifampin was most effective at killing Klebsiella pneumoniae and postponed the bacterial regrowth for 72 hours. The scientists think rifampin temporarily suppresses the antibiotic resistance of Klebsiella pneumoniae, creating the opportunity for the drug trio to kill the bacteria. More testing needs to be done on this combo to prevent regrowth altogether.
"By combining antimicrobials that exert their bacterial killing in different ways, it is possible to outmaneuver the ESKAPE pathogens and completely overwhelm the bacteria's defensive countermeasures," Lenhard said in a press release.
Now that researchers have shown the potential for beating superbugs using sets of triple antibiotics, perhaps the same strategy can be extended to other antibiotic-resistant bacteria that present an urgent threat to global health.
Just updated your iPhone? You'll find new emoji, enhanced security, podcast transcripts, Apple Cash virtual numbers, and other useful features. There are even new additions hidden within Safari. Find out what's new and changed on your iPhone with the iOS 17.4 update.



















Be the First to Comment
Share Your Thoughts