New weapons are needed to combat antibiotic-resistant bacteria. Instead of drugs, scientists have discovered in an animal study that they may be able to harness vampire bacteria to vanquish pneumonia.

As the fish farming industry struggles to become more environmentally friendly, it just gained another problem. Fish food loaded with antibiotic-resistant genes.

Joe McKenna died when he was 30 years old. A young married man with his future ahead of him, he was cleaning up the station where he worked as a fireman. Struck by a piece of equipment fallen from a shelf, Joe complained of a sore shoulder. Over the next week, Joe worsened and ended up in the hospital. Chilled, feverish, and delirious, his organs shut down from an infection we'd now call septic shock.
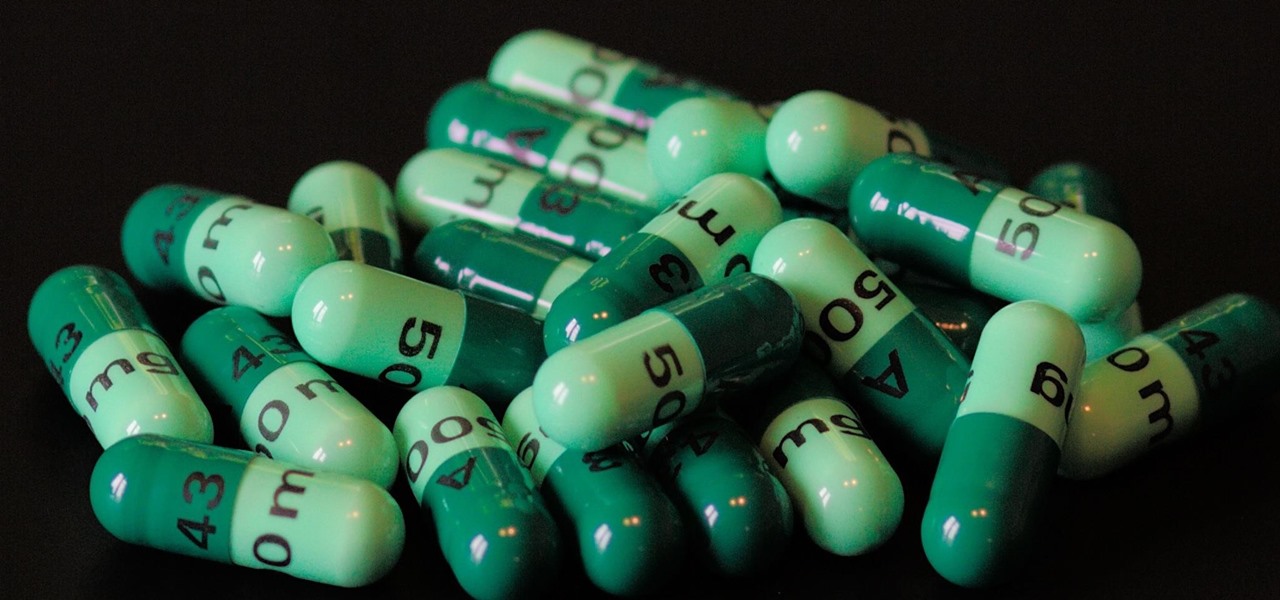
Despite the threat of superbugs, physicians continue to prescribe antibiotics when they might not be needed, and patients are suffering.
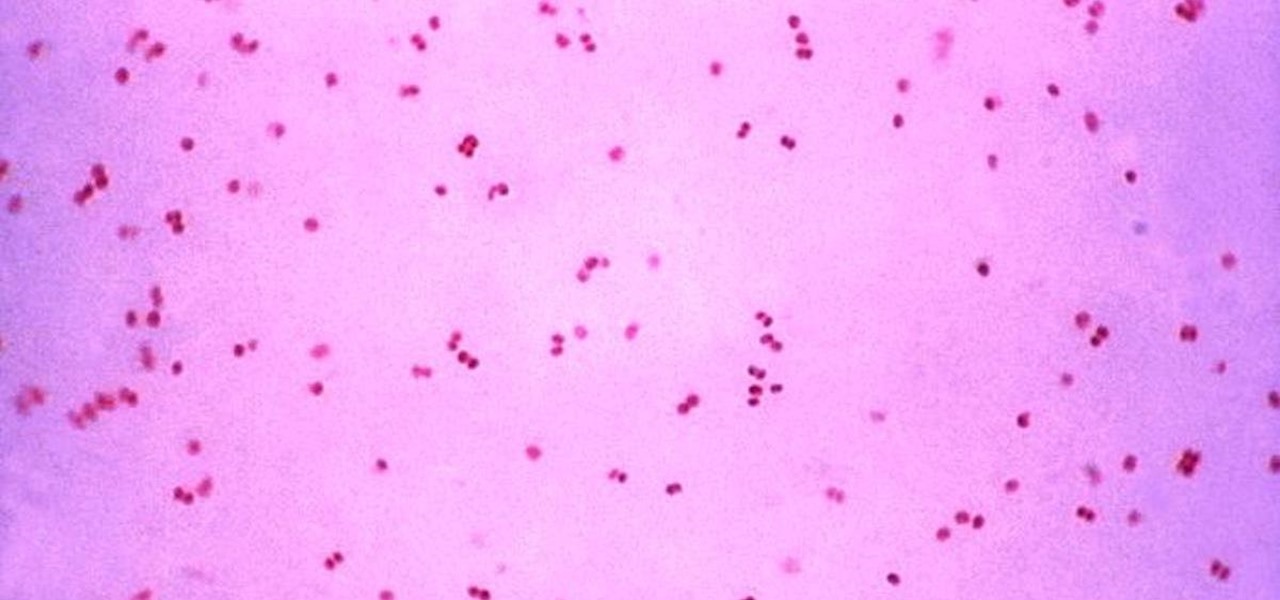
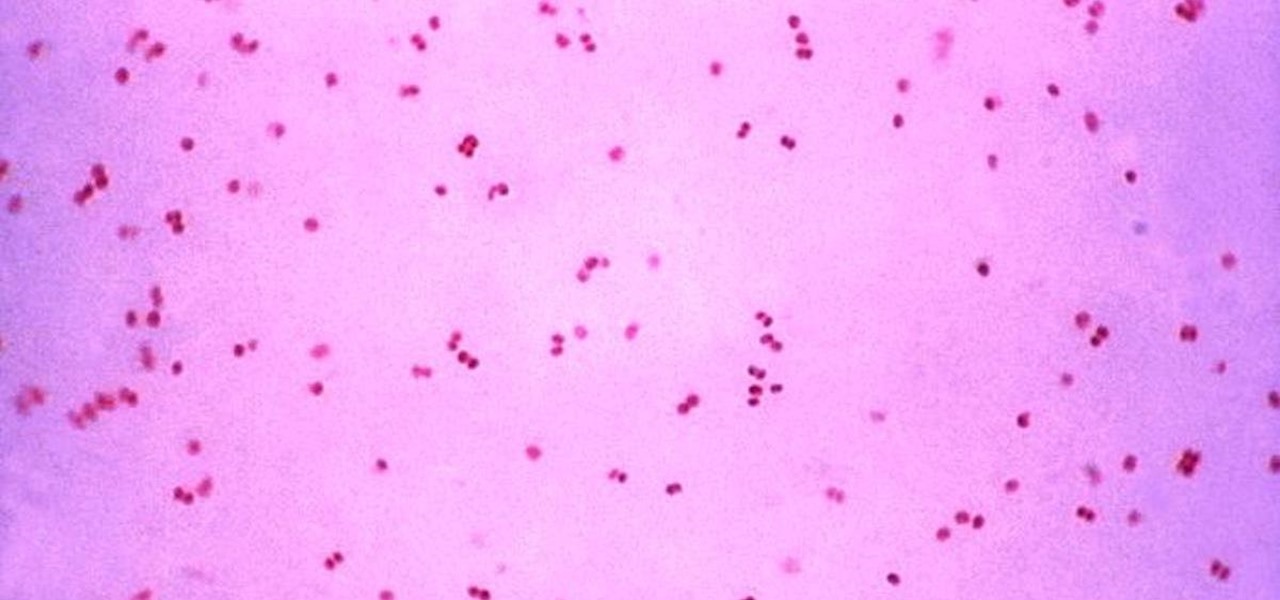
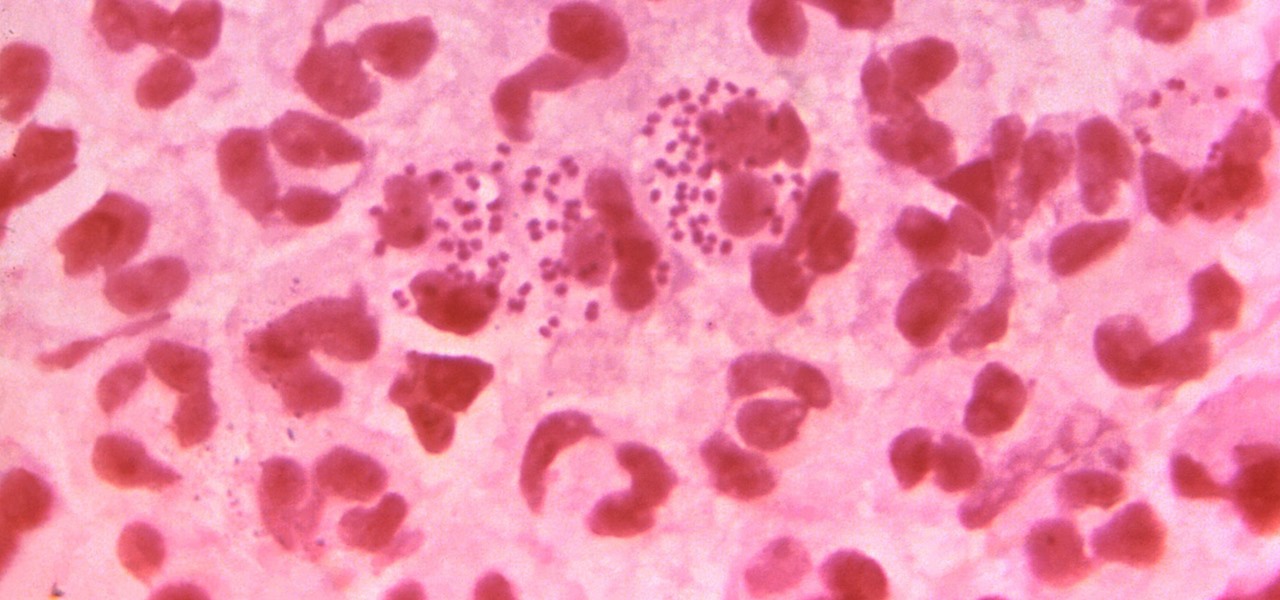
Gonorrhea infections reached a peak in 1975, then decreased until 2009, when infection rate started rising and has increased each year since. With the rise of antibiotic resistance, those numbers are only going to get worse — unless we find new treatments against the bacteria.
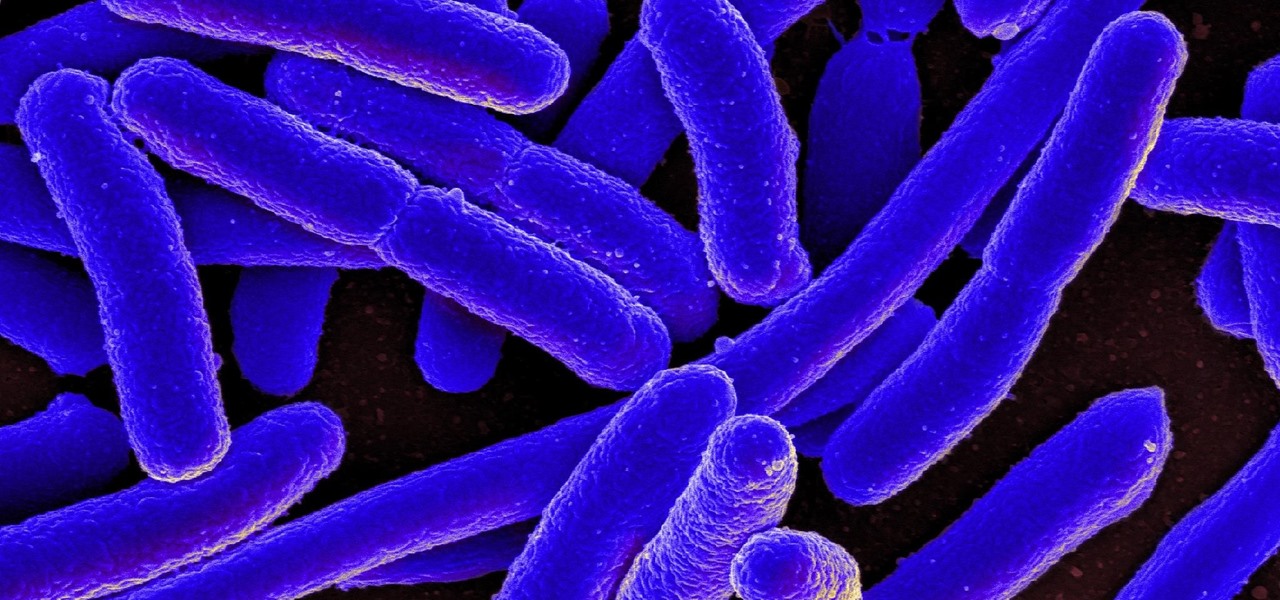
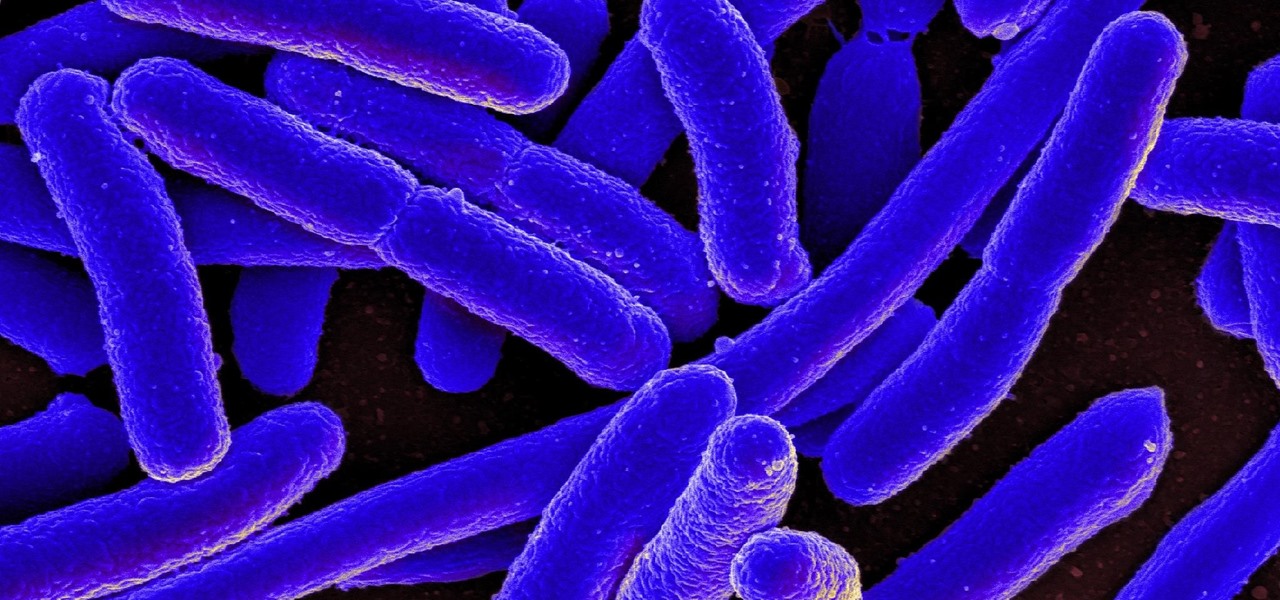
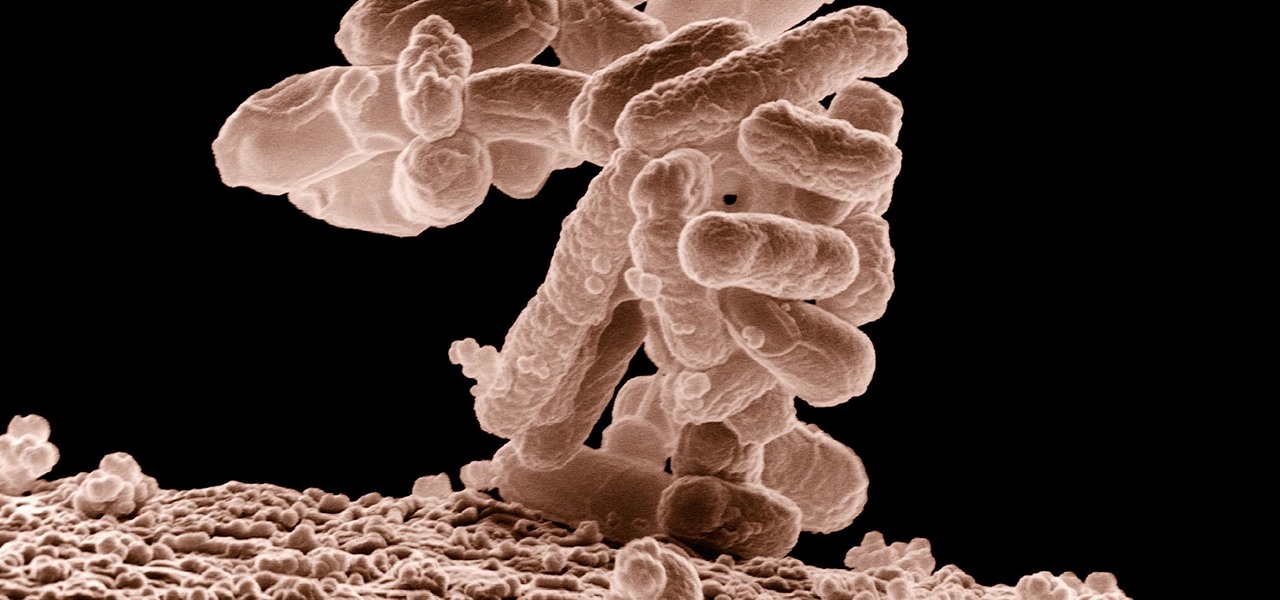
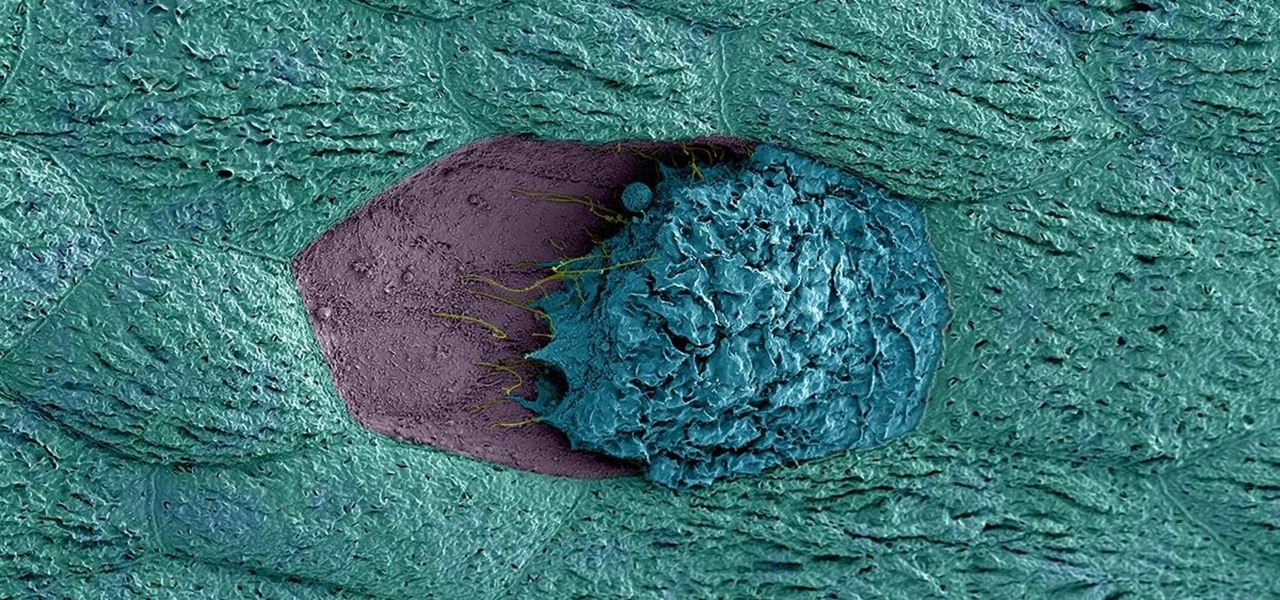
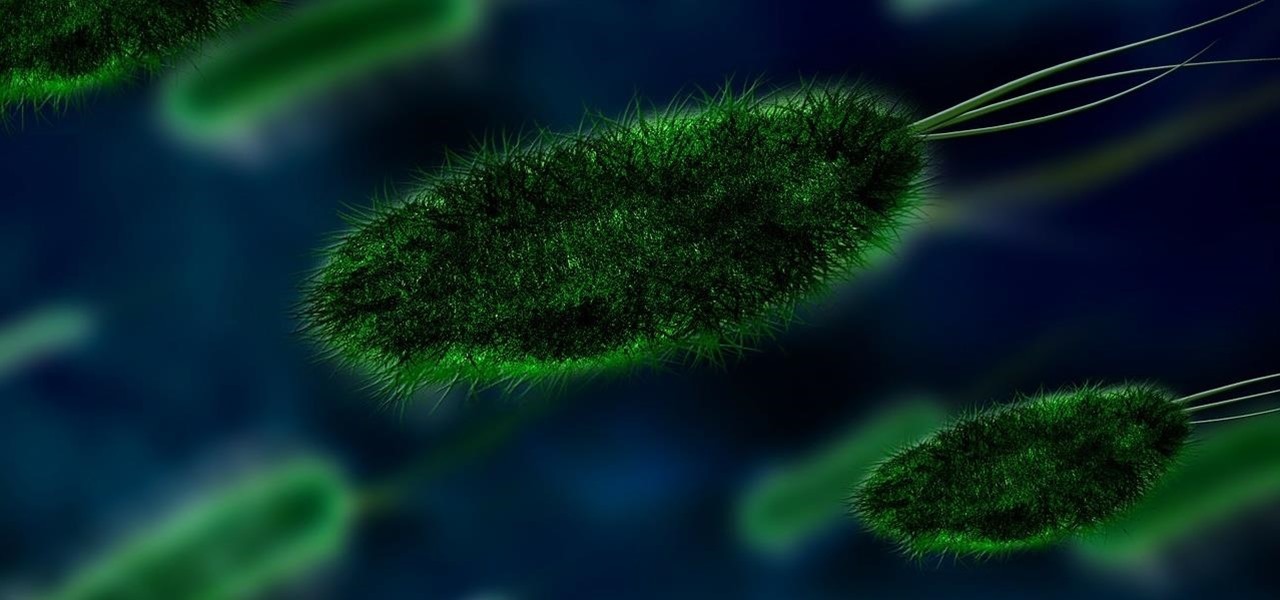
New research reveals how E. coli bacteria construct elaborate and effective tunnels to pump unwanted molecules like antibiotics and other toxins out of cells. The discovery could help us better understand how antibiotic resistance occurs and give us a leg-up to beat them at their own game.

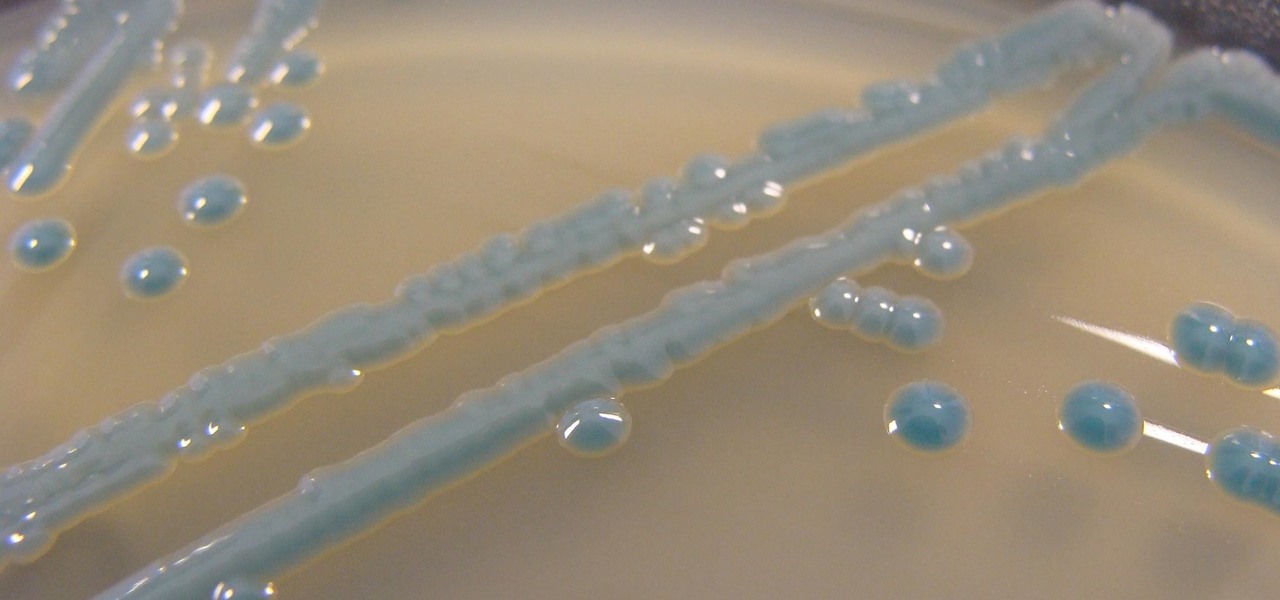
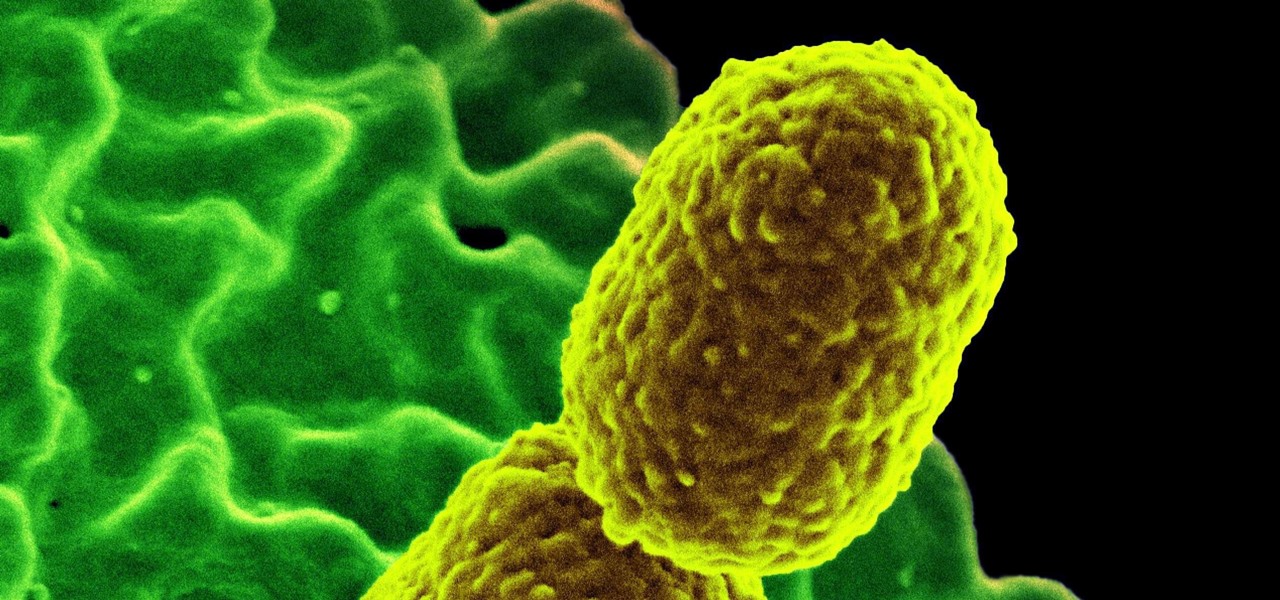
The growing list of dangerous antibiotic resistant organisms has just acquired three new members. Researchers have discovered three new species of Klebsiella bacteria, all of which can cause life-threatening infections and have genes that make them resistant to commonly used antibiotics.

A promising new antibiotic has been discovered in, of all things, another bacteria. Burkholderia bacteria live in diverse habitats, including soil, plants, and humans where they thrive by knocking out other microbes that compete with them for resources or threaten their existence. Scientists have discovered they accomplish this by producing a very effective antibiotic.

Some types of bacterial infections are notoriously tough to treat — and it's not all due to antibiotic resistance. The bacteria themselves are rugged and hard to penetrate with drugs.

Our quest to find new antibiotics has taken a turn — a turn down the road, that is. A team of scientists from the University of Oklahoma is scooping up roadkill and searching for bacteria on them that might yield the world's next antibiotic.

Significant strides have been in the race to find antibiotics to treat superbug infections — those caused by bacteria resistant to the antibiotics used to treat them. Now, an international team of scientists has discovered a new antibiotic produced by a microbe found in Italian soil.

After years of telling patients to finish any prescribed course of antibiotics completely, a group of researchers in the UK say it is no longer necessary, and could even be harmful if we want to preserve the antibiotics we can still use.

The search is on to find antibiotics that will work against superbugs — bacteria that are rapidly becoming resistant to many drugs in our antibiotic arsenal.

Antibiotics used to prevent diseases in livestock are creating a world of hurt for humans and the soil we depend on for food. Bacterial resistance to antibiotics is a global health issue. The overuse, underuse, and poor use of these life-saving drugs is rapidly removing them as a treatment option for serious infections in humans—plus bacteria are naturally adaptive.

One thousand feet under the ground, extremophile microbes that have not seen the light of day for four million years are giving up some fascinating facts to scientists who go the distance.

A terrifying antibiotic-resistant superbug, one thought to only infect hospital patients, has made its debut in the real world. For the first time ever, the superbug carbapenem-resistant Enterobacteriaceae (CRE) infected six people who hadn't been in or around a hospital in at least a year, and researchers aren't sure how they got infected.

A new study has found that up to half of people who think they have a penicillin "allergy" can still receive the drug, and other antibiotics with similar structures, without any negative reactions to the meds. Why? Because they're not really allergic, doctors say.

What do Leo Tolstoy (writer), Beethoven (composer), Paul Gaugin (artist), and Adolf Hitler (politician) have in common? They are all considered to have suffered from the sexually transmitted disease syphilis.

In the race to outsmart "untreatable" antibiotic-resistant gonorrhea, one of the three new treatments on the track is about to enter Phase 3 clinical trials. Hopefully, it'll be widely accessible sooner rather than later, for the 78 million people who are diagnosed with gonorrhea each year.

Although their effectiveness is waning, antibiotics remain a front-line defense against many infections. However, new science reveals using the wrong antibiotic for an infection could makes things much worse.

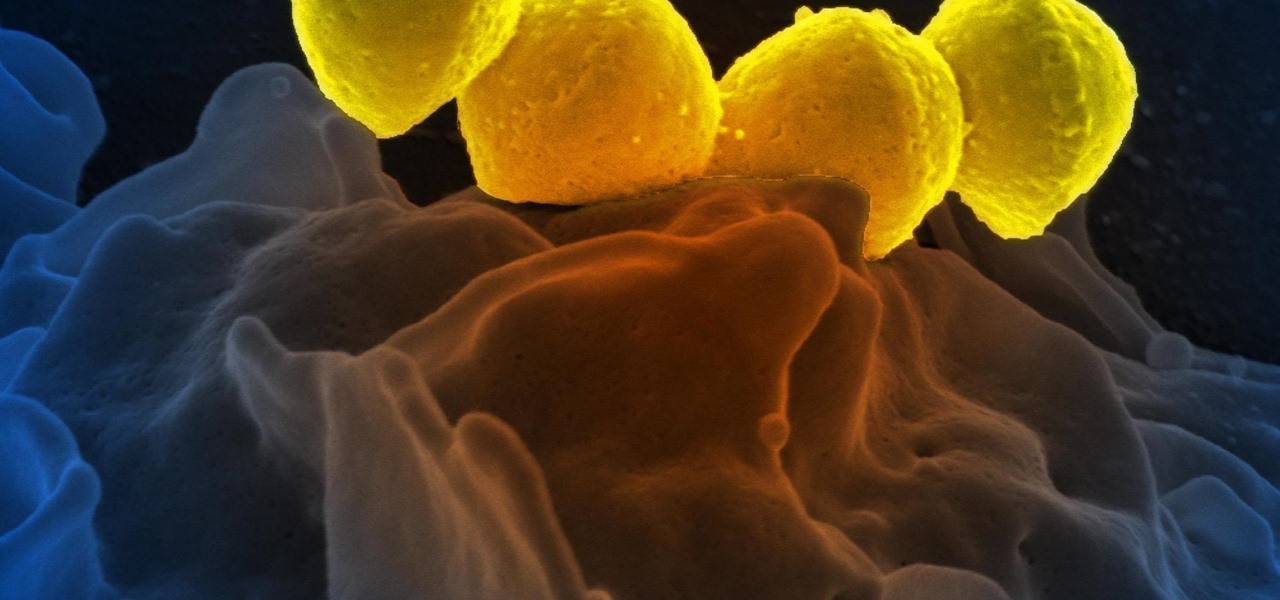
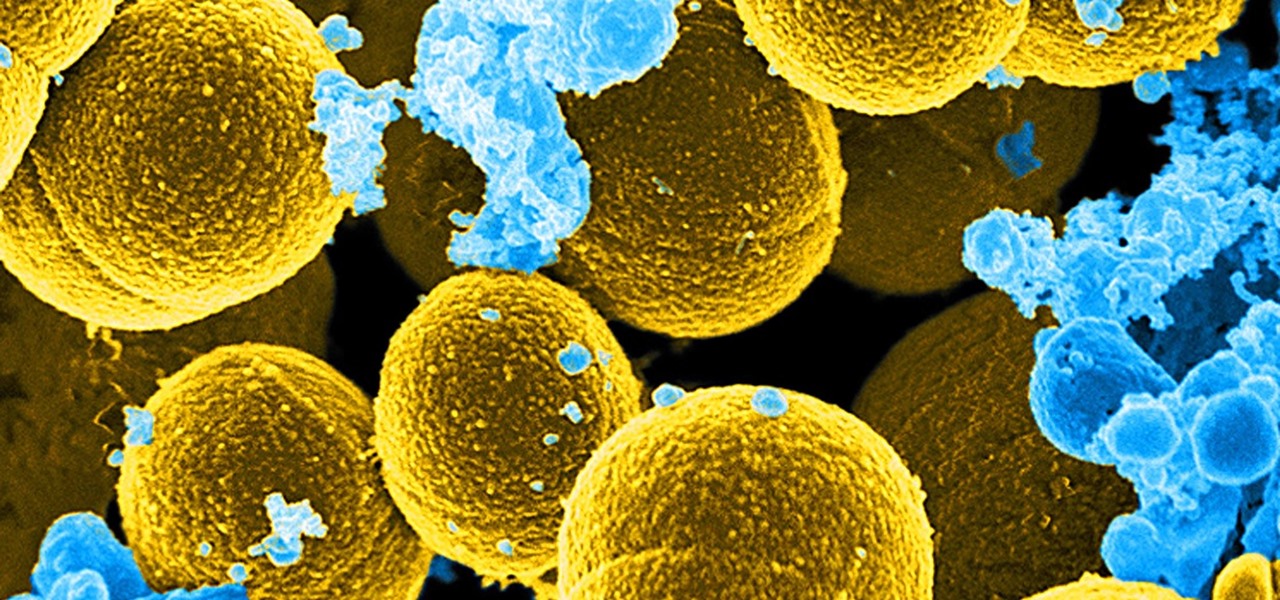
For once there is good news — surprising news, but good news — in the fight against antibiotic-resistant organisms. A recent study found that Staphylococcus aureus bacteria is becoming more sensitive to some key drugs used to treat it.

On October 17, 1943, a story in the New York Herald Tribune read "Many laymen — husbands, wives, parents, brothers, sisters, friends — beg Dr. Keefer for penicillin," according to the American Chemical Society. Dr. Chester Keefer of Boston was responsible for rationing the new miracle drug, penicillin.

Our canine best friends could spread our bacterial worst nightmare, according to a recent study. The problem with drug-resistant bacteria is well known. Overused, poorly used, and naturally adaptive bacteria clearly have us outnumbered. As science drives hard to find alternative drugs, therapies, and options to treat increasingly resistant infections, humans are treading water, hoping our drugs of last resort work until we figure out better strategies.

Add antibiotics to the possible list of culprits responsible for honeybee decline around the world. While it may come as a surprise, antibiotics are commonly mixed into feed used by commercial beekeepers to maintain their hives. In a recent study published in PLOS Biology, researchers from the University of Texas at Austin found antibiotics used to treat honeybees may be a contributing factor in individual bee death and colony collapse.

Antibiotic-resistant infections that usually occur only in hospital settings are spreading in communities, increasing hospital stays—and danger—for young children.

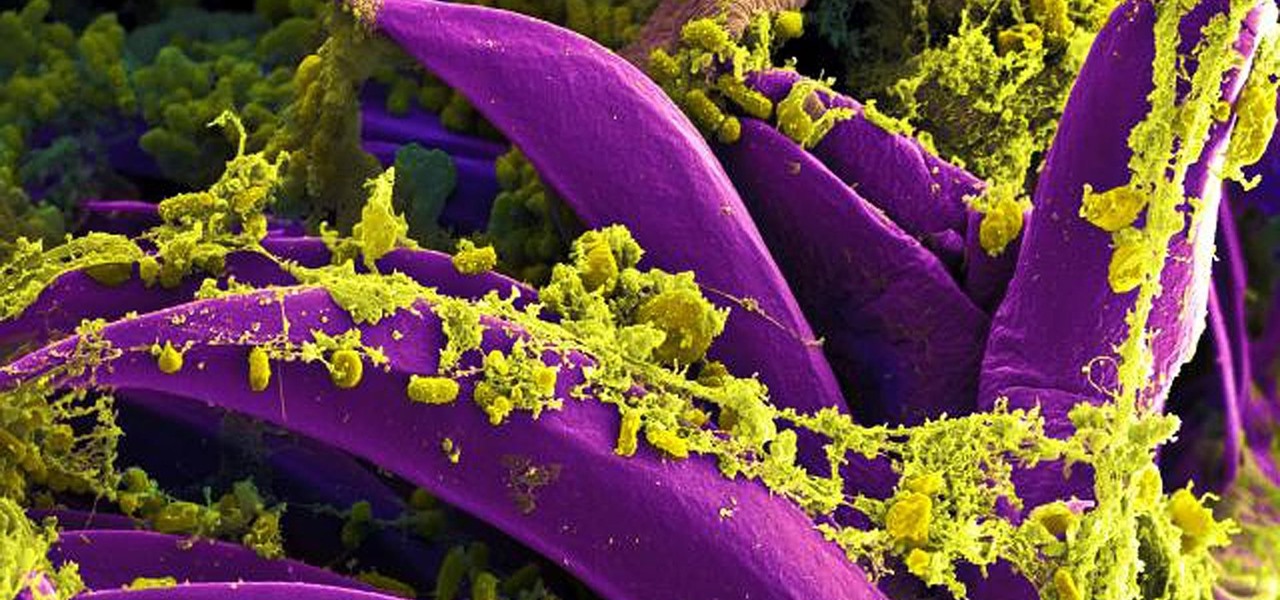
The bacteria Klebsiella pneumoniae is a bad actor known for being antibiotic-resistant and causing a variety of serious infections in hospitals, including pneumonia, surgical site wounds, and meningitis. K. pneumoniae is something you do not want to encounter if you have a compromised immune system.

Urinary tract infections (UTIs) drive over eight million people to seek medical attention every year. Almost all — as many as 90% — of those infections are caused by Escherichia coli. Copper can kill bacteria, but E. coli has found a way to capture the copper, preventing its antibacterial action. Now, researchers have found that, in a cruel irony, the bacteria use the copper it grabs as a nutrient to feed its growth.

Crusty, itchy, red eyes? There is a decent chance you could have conjunctivitis, or pink eye, an infection of the thin lining around the eye and the eyelid, caused by bacteria, an allergen, virus, or even your contact lenses. Whatever the cause — you call up your doctor to get a prescription to clear it up, right? Not really.

In the ongoing search to find better ways to use antibiotics, an extract made from maple syrup has some surprisingly important medical benefits.

Humanity is standing on an infection precipice. As antibacterial resistant grows, we're running out of options, and a recent scary case of total antibiotic resistance is a frighting view of our potential future. In the end, it was septic shock that took the life of a 70-year old woman with an incurable infection. One of few such cases in the US, her death could nonetheless be the shape of things to come.

The noses of kids who live in areas of intense pig farming may harbor antibiotic-resistant bacteria, presumably acquired from the animals, according to a new study by scientists at the Johns Hopkins Bloomberg School of Public Health, UNC Gillings School of Global Public Health, and Statens Serum Institut in Denmark, published in Environmental Health Perspectives.

As researchers from Yale searched our environment for compounds to aid in the battle against drug-resistant bacteria, they got an unlikely assist from ticks.

Antibiotic use in infants has been associated with a host of childhood conditions later in life. Yet when an infection is suspected in a newborn, usually a sample of their blood is drawn to check for the presence of bacteria and 5 to 8 percent of them receive antibiotics while the diagnosis is pending.

The next time you suffer a cut or abrasion, think twice before you reach for the Neosporin. It's time, and mom, tested — you get a cut, you wash it carefully, then apply some triple-threat antimicrobial ointment. You may or may not slap on a band-aid. We won't cover it here, but so that you know, covering the wound with a sterile dressing or band-aid is a good idea.

Yogurt is more than an excellent source of protein, calcium, and gut-healthy probiotic bacteria. A protein isolated from probiotic lactobacillus bacteria in yogurt is capable of inhibiting drug-resistant bacteria.

Antibiotics are one of our main weapons against infections. The problem is that many bacteria are becoming resistant to most of the antibiotics we use to treat them, and those 'superbugs' have created an urgent threat to our global health. A research group found a new way to hit a well known bacterial target and have developed a drug to hit it.

A new study confirms that antibiotics can prevent surgical intervention if your child's appendix becomes inflamed, potentially saving his or her life.

The pathogen referred to as a "nightmare bacteria" is quietly adapting and spreading faster than anticipated.

Most females have had at least one urinary tract infection in their lifetimes. Recurrent UTIs are particularly problematic in young, sexually active women, where about 80% of the infections are caused by the bacteria Escherichia coli, better known as E. coli.

More prescriptions for antibiotics are written for ear infections than any other type of infection. A new study comparing the incidence and causes of ear infections in children between the ages of six months and three years found that the incidence of ear infections over the last decade has dropped significantly since the 1980s.